
Chronic prostatitis is a serious problem. Even modern urology cannot answer many questions about this pathology. Experts believe that chronic prostatitis is a disease caused by a range of health problems, including tissue damage, as well as urinary tract and prostate dysfunction, as well as dysfunction of other organs.
Pathology is mainly diagnosed in males of reproductive age. In older men, chronic prostatitis is often accompanied by benign prostate tumors.
Disease classification
The classification of prostatitis was established in 1995 by scientists at the National Institutes of Health:
%20and%20inflamed%20chronic%20prostatitis%20(right).webp)
- 1 type- Acute bacterial prostatitis. It is diagnosed in 5% of cases of prostate inflammation.
- Type 2- Bacterial chronic prostatitis.
- Type 3- Chronic bacterial prostatitis. This pathology has another name - chronic pelvic pain syndrome.
- Type 3A- Inflammatory forms of chronic prostatitis. 60% of chronic prostatitis cases are diagnosed.
- Type 3B- Non-inflammatory forms of chronic prostatitis. 30% of cases are confirmed.
- Type 4- Asymptomatic prostatitis.
There is also the classification of chronic prostatitis, compiled in 1990.
Symptoms of chronic prostatitis
Pelvic discomfort and pain lasting more than 3 months are the main symptoms of chronic prostatitis.
In addition, urinary disorders and erectile dysfunction were observed:
- Pain occurs in the perineum and can radiate to the anus, groin, inner thighs, sacrum, lower back, and scrotum. On the one hand, the pain extends to the testis, which is often not a symptom of chronic prostatitis;
- No erection occurs despite adequate conditions, but complete impotence has not been observed;
- Premature ejaculation is observed in the early stages of disease development;
- Frequent urination, incontinence, pain, and burning during bladder emptying.
Clinical manifestations may vary depending on the type of chronic prostatitis.
infectious form:
- frequent urination at night;
- Pain in the thighs, perineum, glans, and rectum, aggravated by exercise;
- painful urination;
- Urine flow is weak.
Specific infection:
- urethral mucus discharge;
- above symptoms.
Non-infectious prostatitis:
- Acute pain in the perineum;
- pain in the thigh and head of the penis;
- Pain can increase with forced interruptions in sexual intercourse or a chronic lack of intimacy.
important!The disease develops in waves. Symptoms may diminish or worsen, but their presence clearly indicates the presence of an inflammatory process.
Symptoms may vary depending on the stage of pathological development.

The following developmental stages of pathology are distinguished:
- exudate.Patients experience pain in the pubic, groin, and scrotum. Frequent urination and discomfort after sex. An erection can hurt.
- choose.The pain is intensified and is located in the groin, the pubic part and spreads to the sacrum. Urination is accelerated but not difficult. Erection is not affected.
- proliferative.During exacerbations, urination becomes more frequent. Weak urine flow.
- Keloid.Sclerosis of prostate tissue occurs. There is a feeling of heaviness in the sacral and pubic regions. Increased urination. Erections become weaker. Ejaculation may be completely absent.
Symptoms may vary depending on the course of the disease, but they tend to get progressively worse anyway.
Causes of chronic prostatitis
There are many factors that lead to chronic prostatitis. The disease occurs under the influence of an infectious agent. The patient suffered from hormonal, autonomic, immunological and hemodynamic disturbances. Biochemical factors, urinary reflux into the prostate lobe, and impaired function of growth factors responsible for the proliferation of viable cells can all be affected.
Causes affecting the formation of pathology:
- Genitourinary infection;
- Lack of motivation;
- irregular sex life;
- Continuous catheterization of the bladder;
- Periodic low temperature.
developbacterial diseasePromotes urinary reflux in the prostate.
chronic nonbacterial prostatitisIt develops in the context of neurogenic disorders of the pelvic floor muscles and elements responsible for the function of the bladder wall, prostate and urethra.
formmyofascial trigger pointLocated near the organs of the genitourinary system and prostate, it can cause pelvic pain syndrome. Certain diseases, surgical interventions, and injuries to acupuncture points can cause pain in the pubic area, perineum, and adjacent areas.
pathological diagnosis
The presence of complex symptoms makes the diagnosis of chronic prostatitis easy. However, in some cases, the pathology may be asymptomatic. In this case, in addition to standard examination and questioning of patients, additional research methods are required.Neurological examinations and studies of the patient's immune status must be performed..
important!Specialized questionnaires and questionnaires allow you to more accurately judge the patient's subjective feelings, and comprehensively understand the patient's health status, pain intensity, ejaculation, erection and urination disorders.
laboratory diagnosis
Laboratory diagnosis can differentiate between bacterial and non-bacterial forms of pathology, as well as determine the type of pathogen and make the most accurate diagnosis.Chronic inflammation of the prostate was confirmed when a fourth urine or prostate secretion sample contained more than 10 leukocytes or bacterial associations in the PZ.When the number of white blood cells increases but bacteria are not seeded, inspect the material for chlamydia or other STD pathogens.
- The discharge from the urethra is sent to a laboratory to test it for viruses, fungal and bacterial flora, white blood cells and mucus.
- Scraping from the urethra is checked by PCR. This allows you to identify sexually transmitted pathogens.
- Microscopic examination of prostate secretions to count macrophages, leukocytes, amyloid, and Trousseau-Lallemand bodies. Prescribes the conduct of immunological studies and bacteriological studies. Determine the level of nonspecific antibodies.
- Blood samples were taken ten days after the digital rectal examination to determine the concentration of PSA in it. At rates above 4. 0 ng/ml, patients underwent prostate biopsy to rule out tumor.
Diagnoses are made public based on research findings.
Instrument diagnosis

Defining the stage and form of the disease will facilitate transrectal ultrasound of the glands. Ultrasound allows you to rule out other diagnoses, monitor the effectiveness of treatment, and determine the size of the prostate, its echogenic structure, and the homogeneity and density of the seminal vesicles. Urodynamic studies and electromyography of the pelvic floor muscles will allow to reveal subvesical obstructions and neurogenic disorders that often accompany pathology.
Tomography and MRI are used for differential diagnosis, especially prostate cancer. These methods will reveal invasion of pelvic organs and spine.
Differential diagnosis
Differential diagnosis is important because patients have the potential to develop more severe disease.
A differential diagnosis is established with the following diseases:
- Pseudodysfunction, detrusor-sphincter system dysfunction, neurogenic bladder dysfunction, complex regional pain syndrome;
- Bladder stenosis, hypertrophic changes in the bladder neck, prostate adenoma;
- Osteitis of the pubic joint, cystitis;
- Rectal Pathology.
If symptoms occur, the prostate should be examined by a urologist or andrologist. Perform an ultrasound scan. If necessary, a prostate biopsy is performed.
pathological treatment
Chronic prostatitis treated by a urologist or andrologist. Treatment is performed in a complex manner. Correction depends on the patient's lifestyle, thinking characteristics and habits. It's important to exercise more, minimize alcohol intake, quit nicotine addiction, eat right, and normalize your sex life. However, it will not work without basic treatment. Taking medication is the main condition for full recovery.
Indications for hospitalization
In most cases, treatment is performed on an outpatient basis. But in cases where the disease is uncorrectable and prone to relapse, patients are referred to hospitals where treatment is more effective.
medical treatment
This approach is designed to eliminate existing infections, normalize blood circulation, improve drainage of the prostate lobules, correct hormonal background and immune status. Therefore, doctors prescribe antibiotics, vasodilators, immunomodulators, anticholinergics, and anti-inflammatory drugs.
Antibiotics are definitely recommended if the pathology is bacterial in nature. This medication is prescribed based on bacterial cultures of prostate secretions.This will make it possible to isolate pathogens and subsequently determine their susceptibility to specific drugs. Well-designed programs, the treatment efficiency of more than 90%.
In the non-bacterial form, short-term antibiotics are prescribed. It will continue only if the program gives positive results. The effective rate of treatment is about 40%
For chronic pelvic pain, the duration of a course of antibiotics should not exceed one month. Under positive dynamics, treatment will continue for one month. If it doesn't work, switch to another medicine that may be more effective.
Fluoroquinolone antibacterials are the mainstay of treatment of pathology.They are highly bioavailable, active against most Gram-negative bacteria, Ureaplasma and Chlamydia, and accumulate in prostate tissue.
Penicillin may be prescribed when fluoroquinolone therapy is ineffective.
Antimicrobials are used for prophylactic purposes.
After treatment with antibiotics, it is treated with alpha-blockers.This treatment strategy is effective in patients with persistent obstruction and irritation.
If urination disturbance and pain persist, tricyclic antidepressants with analgesic properties may be prescribed.
For severe voiding disorders, before initiating treatment, conduct a urodynamic study and act on the results obtained.
non-drug treatment
Non-drug treatments can increase the concentration of antimicrobials in glandular tissue, but exceeding doses is not recommended.
For this, the following methods are used:
- electrophoresis;
- Laser Treatment;
- Acoustic swimming;
- Microwave hyperthermia (transrectal application).
When the latter method is applied, the temperature is selected individually. The temperature is set in the range of 39-40 degrees, allowing you to increase the concentration of the drug in your body, activate the immune system at the cellular level, eliminate bacteria and relieve congestion. Increasing the range to 40-45 degrees can achieve a stiffening and analgesic effect.
A combination of laser and magnetic therapy is used. The effect is similar to that of the above method, but also has a biostimulating effect on the organ.
Transrectal massage is performed only in the absence of contraindications.
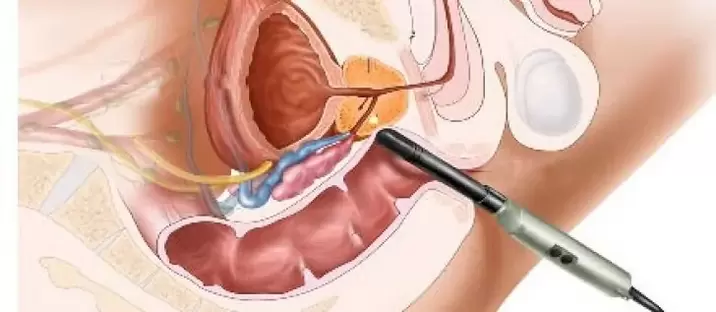
Surgical approach
Chronic prostatitis generally does not require surgery. Complications that threaten the health and life of the patient are excluded. Modern surgical treatment allows the use of endoscopic surgery. It is minimally invasive. Recovery is faster with minimal damage to the body.
Surgical methods are prescribed for:
- Sclerosis of the prostate;
- prostate adenoma;
- hardened seed nodules;
- Prostate calcification.
important!Surgery is contraindicated in the acute phase. Surgical treatment is prescribed by the surgeon based on the findings of the study and the overall clinical situation.
Prognosis of chronic prostatitis
Doctors are cautious about predicting the outcome of a disease. It is difficult to fully recover. Basically, chronic prostatitis enters a long-term remission phase. Symptoms disappeared and urine and blood counts returned to normal. In order that chronic prostatitis does not become more active and does not cause complications, it is necessary to follow all the advice of experts.

























